There are several reasons for a patient to require the implant of a venous access port. If a vascular access will be needed for longer than a 6 week period, an implanted port is highly recommended. The procedure for implanting the venous access port is done in the operating room. Treatments such as chemotherapy, total parenteral nutrition or long term antibiotics, which need to be given to the patient on a regular basis, requires a stable venous access. In addition to these treatments, frequent blood samples will be required to be drawn. The Huber needle, is what is used to access these implanted ports.
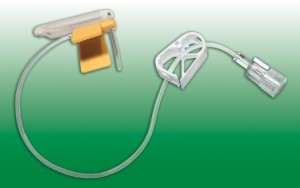
The Huber needle is a hollow needle with a beveled tip. The implanted venous access is under the skin and this needle makes it easy to go through the skin and the silicon septum of the port. These needles come in different sizes in order to accommodate the size of the patient and the port. The use of the Huber needle, prevents the patient from having to endure many needle sticks, because the needle is left in the port for more than one use.
The Huber needles come straight or curved. When the port is only needing to be flushed, the straight needle is used. These are also used for any short-term application. The curved needles are the ones that are used for the delivery of such things as, medications, nutritional fluids, and chemotherapy. The curved needle is convenient, because it can be left in place for a few days, according to the policy of the facility and prevents the patient from having as many needle sticks.
The history behind the Huber needle, may be a slight bit surprising. This widely used needle was actually invented by a dentist in Seattle. He made the needle hollow and curved, making it more comfortable for his patients to endure injections. The Huber needle is today, the only needle that is used to access the implanted venous access port devices.
Most of the patients that have conditions requiring an implanted venous access port, have to have blood drawn several times a day. After a short period of time, their veins collapse. With the use of the implanted port and the Huber needles, the job can be done without having to go through the skin every time.
The Huber needle is safe and can be kept in place for several days. It makes life a lot better for the patient. The reality of having chemotherapy and being stuck so many times in a day, is made a slight bit easier by its use. The administration of the chemotherapy often damages the skin and tissues around peripheral insertion sites. A port that is surgically inserted in the chest wall, helps the patients by only having to endure one needle stick versus many.
Proper use of the Huber needle protects the patient from pain and infection. Huber needles optimize access to the port through the septum of the implanted port. The fluid flows through the reservoir of the port into the vascular system of the patient. Every facility has policies and procedures for the use of the Huber needles, be familiar with them and always follow the regulations.